Levodopa and antisaccade performance in Parkinson’s disease: the influence of intrinsic dopaminergic functioning, dopamine agonists and chronic anti-parkinsonian medication
Dublin Core
Title
Levodopa and antisaccade performance in Parkinson’s disease: the influence of intrinsic dopaminergic functioning, dopamine agonists and chronic anti-parkinsonian medication
Creator
Amy Austin
Date
14th September 2022
Description
The antisaccade (AS) task is a validated eye-tracking paradigm primarily used to assess response inhibition. Although several studies have established AS error rate and latency to be increased in Parkinson’s disease (PD), the evidence regarding the effect of existing anti-parkinsonian medication (e.g., levodopa) on these parameters is contradictory. According to the dopamine overdose hypothesis (DOH), the effect of levodopa on AS performance should be dependent upon the intrinsic dopaminergic functioning of the individual. The current study is the first study to use spontaneous eye blink rate (SEBR), a proxy measure for dopamine activity, to investigate the influence of intrinsic dopaminergic functioning on AS performance following levodopa consumption. The influence of additional PD related factors was also examined. SEBR and AS performance was assessed in eleven healthy controls (HC) and nine participants with PD. SEBR and AS performance was assessed twice in participants with PD, once 30 minutes prior to, and once one hour after, the consumption of levodopa. Pre-levodopa consumption SEBR was a significant positive predictor of AS error rate post, but not pre, levodopa consumption. Total years consuming anti-parkinsonian medications was positively predictive of AS error rate both pre and post levodopa consumption. The regular consumption of dopamine agonists was found to significantly predict fewer AS errors following the consumption of levodopa. The current results support the DOH; higher intrinsic dopaminergic functioning was associated with increased AS errors following the artificial stimulation of dopamine via by levodopa. Therefore, artificial dopaminergic stimulation of an intrinsically sufficiently functioning dopaminergic system appears to produce an overstimulation/overdose effect whereby consequential detrimental effects on AS performance/response inhibition are observed. The current findings go some way in explaining the inconsistencies within the literature.
Subject
Keywords: Parkinson’s disease, dopamine overdose hypothesis, spontaneous eye blink rate, levodopa, dopamine agonists, antisaccade
Source
Twenty-one participants, 10 individuals with mild-moderate idiopathic PD (Mage = 67.10, SDage = 8.63) and 11 healthy control older adults of comparable age (HC; Mage = 66.82, SDage = 9.09) were recruited to the study. The mean age of recruited HC and PD individuals did not differ significantly, t (18.95) = - 0.07, p = .943). Participants were recruited via established research databases and via the social network of the researcher. As the current study focused on PD, participants with a diagnosis of any neurological conditions (beyond PD) were excluded. Additionally, as depression and anxiety influence an individual’s saccadic performance profile and SEBR (Jazbec et al., 2005; Mackintosh et al., 1983), individuals who obtained a clinically moderate depression or anxiety score, as measured by the Hospital Anxiety and Depression scale (HADS), were excluded. Similarly, mild cognitive impairment (MCI) and dementia are associated with increased AS error rate and AS latency (Opwonya et al., 2022), and increased SEBR (D’Antonio et al., 2021). As such, those who presented a cognitive profile indicative of MCI/dementia (score < 82 on the Addenbrookes Cognitive Exam-III, ACE-III; Hsieh et al., 2013) were excluded from the current study. Finally, as experimental stimuli in the current study were coloured red and green, individuals with red-green colour vision deficiency, detected via the Ishihara test (Ishihara, 1917) were also excluded.
On these grounds of exclusion, one individual with PD was excluded from the current study due to obtaining an ACE-III score indicative of MCI. Subsequently, nine individuals with mild-moderate idiopathic PD (Mage = 65.89, SDage = 8.21) and eleven HC individuals (Mage = 66.82, SDage = 9.09) participated in the study. All participants had normal or corrected to normal vision.
All participants with PD were classified as Hohen and Yahr stage II or below (Hoehn & Yahr, 1998), indicating they were physically independent and capable of completing all study tasks. At the time of testing, all PD participants were receiving anti-parkinsonian medication (see table 2 for PD sample anti-parkinsonian medication summary). All PD participants were tested under their normal medication regime, that is, participants attended the study 30 minutes prior to the consumption of their next, normally scheduled, dosage of levodopa-based medication. Accordingly, measures were obtained both pre (30 minutes prior) and post (1 hour after) levodopa consumption, permitting the respective investigations of pre and post levodopa consumption SEBR, motor symptom severity, AS performance and PS performance.
An online calculator computed the levodopa equivalent daily dosages (LEDD) for each participant with PD. LEDD indicates the equivalent amount of levodopa an individual receives from all anti-parkinsonian medications across a 24-hour window (Julien et al., 2021). The online calculator can be accessed via: https://www.parkinsonsmeasurement.org/toolBox/levodopaEquivalentDose.htm
Materials and measures
Online questionnaire
A questionnaire comprised of a demographics and health screening survey, the Edinburgh handedness inventory (EHI), the HADS, and a PD and associated medication
survey was developed and distributed via Qualtrics (Qualtrics, 2013). The questionnaire required 15 minutes to complete.
Demographics and health screening survey. Participants were asked to disclose key demographic and health information (e.g., age, sex, whether they had normal or corrected to normal vision). Participants were also asked to disclose any history of visual impairments, neurological conditions (beyond PD), psychiatric illness, or rheumatic illness.
The EHI (Oldfield, 1971). The EHI is a highly reliable (r = .97, p < .001; Oldfield, 1971) and internally consistent (a = 0.88; Oldfield, 1971) self-report measure of an individual’s hand dominance (Edlin et al., 2015). Participants are requested to indicate their typical hand preference, via five-point Likert scales ranging from ‘always left’- ‘always right’, when completing a range of daily activities (e.g., writing). A final score of ≥ 50 indicates right hand dominance, < 50 to > −50 indicates ambidexterity, and ≤−50 indicates left hand dominance. As hand dominance typically corresponds to ocular dominance (McManus et al., 1999), the EHI was used to infer the dominant eye of each participant in the current study. Monocular eye tacking was then conducted on the dominant eye (Ehinger et al., 2019).
The HADS (Zigmond & Snaith, 1983). The HADS is a short self-assessment questionnaire validated to detect anxiety and depression within the general population, inclusive of the elderly (Bjelland et al., 2002). Respondents are required to indicate, via four- point Likert scales, how 14 items relate to their recent feelings. Responses range from ‘0’ (the item has little relevance to recent feelings), to ‘4’ (the item is significantly representative of recent feelings). Likert responses are summed separately for anxiety and depression relevant items. Scores of seven or less indicate no notable presence of anxiety and depression. Scores ranging between eight and 10 indicate mild levels, between 11 and 14 indicate moderate levels, and between 15 and 21 indicate severe levels.
PD and associated medication survey. Individuals with PD were asked to disclose further health information regarding the number of years since their PD diagnosis, which anti-parkinsonian medications they were currently receiving, the daily dosages of these medications and the total number of years they had been consuming anti-parkinsonian medications.
ACE-III (Hsieh et al., 2013)
The ACE-III is a well validated (Hseih et al., 2013), highly reliable and internally consistent (ICC = 0.92, a = 0.87 respectively; Takenoshita et al., 2019) cognitive assessment used to screen for the presence of MCI and dementia syndromes (Hsieh et al., 2013). To provide a global neuropsychological evaluation, participants are asked to complete tasks assumed to relate to five principal cognitive functions, namely: memory, language, attention, visuospatial skills, and verbal fluency (Hodges & Larner, 2017). Scores ascertained from each of the five domains are summed and the individual receives an overall score relative to the maximum possible score of 100. Higher scores indicate better cognitive functioning. A score below 82 is indicative of cognitive impairment.
Ishihara colour deficiency test (Ishihara, 1917)
The Ishihara colour deficiency test is a 38-item assessment of red-green colour perception. Typical red-green colour vision is marked by the ability to correctly decipher a number or pattern embedded within 38 red/green circular images. The test requires three minutes to complete.
MDS-UPDRS (Goetz et al., 2008)
Both motor and non-motor PD symptoms were evaluated using the MDS-UPDRS. The MDS-UPDRS is comprised of four distinct subscales. Subscale I focuses on non-motor symptoms associated with PD (e.g., cognitive impairment, dopamine dysregulation syndrome), whereas subscales II – IV focus on the motor symptoms associated with PD. Subscales I, II and IV require participants to retrospectively respond with answers reflecting their average symptoms/experiences over the previous week. Whereas subscale III directly assesses current functioning via a motor exam. The motor examination requires participants to perform a series of motor tasks (e.g., finger tapping, walking, arising from a chair) under the observation of the examiner. The examiner rates the severity of motor impairment displayed during each motor task performed. All subscales of the MDS-UPDRS are scored according to four-point-Likert scales whereby ‘0’ indicates no impairment and ‘4’ indicates the most severe impairment. Hoehn and Yahr (Hoehn & Yahr, 1998) stages were calculated based upon the MDS-UPDRS assessment. The accumulative score of subscales I, II, III and IV provide an overall MDS-UPDRS score indicative of PD severity. A maximum score of 199 is reflective of the most severe disability the result of PD (Holden et al., 2018). The MDS-UPDRS requires approximately 30 minutes to complete.
SEBR
SEBR was assessed by recording participant’s eye movements whilst sitting at rest. The recording device was located approximately 55cm directly in front of the participant. Participants were not informed that they were completing an assessment of their blink rate, nor were they engaged into conversation with the examiner as both informing participants that their blink rate is being assessed and conversing increase SEBR (Doughty, 2001). Participants eye movements were recorded for two-and-a-half minutes however, only the last one minute of each recording was coded for SEBR (one minute is sufficiently long enough to obtain a representative blink rate, Deuschl & Goddemeier, 1998). A blink was identified (and coded accordingly) as full eye lid closure which was the result of bilateral movement of the eyelids (Kimber & Thompson, 2000). SEBR was scored as the number of blinks per minute. PD participant pre-levodopa consumption SEBR was considered their baseline SEBR, reflective of intrinsic dopaminergic functioning (Kimber & Thompson, 2000).
Eye tracking tasks
Apparatus
A desktop mounted eye tracker (Eyelink Desktop 1000), operating in monocular mode, with a sampling rate of 500 Hz was used to record eye movements of the participant’s dominant eye. An adjustable chin rest with attached forehead rest was utilized to minimise head movements. The eye tracking camera was located at the base of the stimuli presenting computer monitor. Participants sat approximately 55cm away from the eye tracking camera and computer monitor. A 4-point calibration, whereby participants are asked to fixate upon a red circle as it moves from the top, bottom, right and left side of the computer screen, was used prior to the commencement of all eye tracking tasks. Frequent calibration improves the accuracy of eye-tracking data (Pi & Shi, 2019). All eye tracking tasks were developed and operated using experiment builder software version 1.10.1630. Habitual eye glass wearers were not required to remove their eyeglasses during eye tracking tasks. Eye tracking tasks required approximately 10 minutes to complete.
Prosaccade task
Participants completed four practice trials and 16 experimental gap trials. To centre a participant’s gaze at the start of each trial, a white fixation stimulus was presented for 1000 milliseconds (ms) in the centre of a back computer screen. A red lateralised target was then displayed randomly either to the right or the left of the central fixation for 1200ms at 4 ° eccentricity. The PS task operated according to the gap paradigm. Accordingly, to create a temporal gap between fixation and target stimuli, a black interval screen was presented for 200ms between the extinguishing of the white fixation stimulus and the presentation of the red target stimulus. For the PS task, participants were instructed to shift their visual focus towards the location of the red target as quickly and as accurately as possible.
Antisaccade task
Participants completed four practice trials followed by 24 experimental gap trials. Participants were presented with a white central fixation stimulus on a black computer screen for 1000ms. Following a 200ms black interval screen, a green lateralised target stimulus was presented at random to either the left or right of the central fixation. The green target was displayed for 2000ms at 4 ° eccentricity. Participants were instructed to shift their visual focus to the opposite direction of where the green target stimulus appeared. An example of a successful trial would be as follows, if the green target stimulus was presented left-lateralised, participants should direct their gaze to the right side of the computer screen.
Procedure
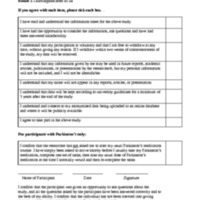
The present study was reviewed and approved by Lancaster University’s ethics committee. All participants provided informed consent prior to participating.
Participants were tested on one day and testing sessions took no longer than two hours. Individuals with PD completed SEBR assessments, MDS-UPDRS III motor examinations and all eye tracking tasks twice, once 30 minutes prior to consuming their usually scheduled dosage of levodopa medication, and once again one hour following the consumption of their levodopa medication. Prior research indicates that one hour is sufficient for levodopa to be metabolized and produce therapeutic effects (Lu et al., 2019). This method of testing the effect of anti-parkinsonian medications is widely used within the literature and no detrimental effects of this method have been reported (Cools et al., 2003). Similarly, re- test on the PS and AS tasks does not significantly influence performance (Larrison-Faucher et al., 2004). HC participants completed all study tasks once.
All participants completed the online questionnaire 48 hours prior to attending testing sessions. Upon arriving to testing, all participants completed an assessment of SEBR followed by the PS and the AS tasks. HC participants then completed the ACE-III and the Ishihara test. HC participation in the study was then complete. PD participants continued with further testing. Specifically, PD participants then completed the MDS-UPDRS subscale III motor examination. PD participants then consumed their usual dose of levodopa medication at their usual time. During the one-hour levodopa metabolization period, participants with PD completed subscales I, II and IV of the MDS-UPDRS, the ACE-III and the Ishihara test.
Once one hour had elapsed, individuals with PD then re-completed an assessment of SEBR, the PS and the AS task, and were also re-assessed via the MDS-UPDRS subscale III motor examination. Thus, motor symptom severity (MDS-UPDRSIII), SEBR and eye- tracking data were obtained from both pre (baseline) and post levodopa consumption medication states.
Data processing
Raw data were extracted via EyeLink using DataViewer Software Version 3.2 and processed offline using the bespoke software SaccadeMachine (Mardanbegi et al., 2019). SaccadeMachine removes noise and spikes within the data; frames with a velocity signal greater than 1500 deg/s or with an acceleration signal greater than 100,000deg2/sec are filtered out. Fixations and saccadic events were detected via the EyeLink Parser. Trials were excluded where participants failed to direct their gaze to the central fixation stimulus. To ensure saccadic data were reflective of responses to target presentation, a temporal window of 80-700ms from the initial onset of the target stimulus was used (i.e., anticipatory saccades produced prior to 80ms, and excessively delayed saccades produced after 700ms were excluded). The following variables were extracted from the processed data: PS latency (the time taken between the onset of the target stimulus and the first correct fixation), PS error rate (the number of times the participant failed to generate a reflexive saccade to fixate upon the target stimulus), AS latency (the time taken between the onset of the target stimulus and the first correct fixation in the opposite direction to the target stimulus), AS error rate (the number of times a participant erroneously performed a reflexive PS towards the novel target stimulus instead of looking away).
On these grounds of exclusion, one individual with PD was excluded from the current study due to obtaining an ACE-III score indicative of MCI. Subsequently, nine individuals with mild-moderate idiopathic PD (Mage = 65.89, SDage = 8.21) and eleven HC individuals (Mage = 66.82, SDage = 9.09) participated in the study. All participants had normal or corrected to normal vision.
All participants with PD were classified as Hohen and Yahr stage II or below (Hoehn & Yahr, 1998), indicating they were physically independent and capable of completing all study tasks. At the time of testing, all PD participants were receiving anti-parkinsonian medication (see table 2 for PD sample anti-parkinsonian medication summary). All PD participants were tested under their normal medication regime, that is, participants attended the study 30 minutes prior to the consumption of their next, normally scheduled, dosage of levodopa-based medication. Accordingly, measures were obtained both pre (30 minutes prior) and post (1 hour after) levodopa consumption, permitting the respective investigations of pre and post levodopa consumption SEBR, motor symptom severity, AS performance and PS performance.
An online calculator computed the levodopa equivalent daily dosages (LEDD) for each participant with PD. LEDD indicates the equivalent amount of levodopa an individual receives from all anti-parkinsonian medications across a 24-hour window (Julien et al., 2021). The online calculator can be accessed via: https://www.parkinsonsmeasurement.org/toolBox/levodopaEquivalentDose.htm
Materials and measures
Online questionnaire
A questionnaire comprised of a demographics and health screening survey, the Edinburgh handedness inventory (EHI), the HADS, and a PD and associated medication
survey was developed and distributed via Qualtrics (Qualtrics, 2013). The questionnaire required 15 minutes to complete.
Demographics and health screening survey. Participants were asked to disclose key demographic and health information (e.g., age, sex, whether they had normal or corrected to normal vision). Participants were also asked to disclose any history of visual impairments, neurological conditions (beyond PD), psychiatric illness, or rheumatic illness.
The EHI (Oldfield, 1971). The EHI is a highly reliable (r = .97, p < .001; Oldfield, 1971) and internally consistent (a = 0.88; Oldfield, 1971) self-report measure of an individual’s hand dominance (Edlin et al., 2015). Participants are requested to indicate their typical hand preference, via five-point Likert scales ranging from ‘always left’- ‘always right’, when completing a range of daily activities (e.g., writing). A final score of ≥ 50 indicates right hand dominance, < 50 to > −50 indicates ambidexterity, and ≤−50 indicates left hand dominance. As hand dominance typically corresponds to ocular dominance (McManus et al., 1999), the EHI was used to infer the dominant eye of each participant in the current study. Monocular eye tacking was then conducted on the dominant eye (Ehinger et al., 2019).
The HADS (Zigmond & Snaith, 1983). The HADS is a short self-assessment questionnaire validated to detect anxiety and depression within the general population, inclusive of the elderly (Bjelland et al., 2002). Respondents are required to indicate, via four- point Likert scales, how 14 items relate to their recent feelings. Responses range from ‘0’ (the item has little relevance to recent feelings), to ‘4’ (the item is significantly representative of recent feelings). Likert responses are summed separately for anxiety and depression relevant items. Scores of seven or less indicate no notable presence of anxiety and depression. Scores ranging between eight and 10 indicate mild levels, between 11 and 14 indicate moderate levels, and between 15 and 21 indicate severe levels.
PD and associated medication survey. Individuals with PD were asked to disclose further health information regarding the number of years since their PD diagnosis, which anti-parkinsonian medications they were currently receiving, the daily dosages of these medications and the total number of years they had been consuming anti-parkinsonian medications.
ACE-III (Hsieh et al., 2013)
The ACE-III is a well validated (Hseih et al., 2013), highly reliable and internally consistent (ICC = 0.92, a = 0.87 respectively; Takenoshita et al., 2019) cognitive assessment used to screen for the presence of MCI and dementia syndromes (Hsieh et al., 2013). To provide a global neuropsychological evaluation, participants are asked to complete tasks assumed to relate to five principal cognitive functions, namely: memory, language, attention, visuospatial skills, and verbal fluency (Hodges & Larner, 2017). Scores ascertained from each of the five domains are summed and the individual receives an overall score relative to the maximum possible score of 100. Higher scores indicate better cognitive functioning. A score below 82 is indicative of cognitive impairment.
Ishihara colour deficiency test (Ishihara, 1917)
The Ishihara colour deficiency test is a 38-item assessment of red-green colour perception. Typical red-green colour vision is marked by the ability to correctly decipher a number or pattern embedded within 38 red/green circular images. The test requires three minutes to complete.
MDS-UPDRS (Goetz et al., 2008)
Both motor and non-motor PD symptoms were evaluated using the MDS-UPDRS. The MDS-UPDRS is comprised of four distinct subscales. Subscale I focuses on non-motor symptoms associated with PD (e.g., cognitive impairment, dopamine dysregulation syndrome), whereas subscales II – IV focus on the motor symptoms associated with PD. Subscales I, II and IV require participants to retrospectively respond with answers reflecting their average symptoms/experiences over the previous week. Whereas subscale III directly assesses current functioning via a motor exam. The motor examination requires participants to perform a series of motor tasks (e.g., finger tapping, walking, arising from a chair) under the observation of the examiner. The examiner rates the severity of motor impairment displayed during each motor task performed. All subscales of the MDS-UPDRS are scored according to four-point-Likert scales whereby ‘0’ indicates no impairment and ‘4’ indicates the most severe impairment. Hoehn and Yahr (Hoehn & Yahr, 1998) stages were calculated based upon the MDS-UPDRS assessment. The accumulative score of subscales I, II, III and IV provide an overall MDS-UPDRS score indicative of PD severity. A maximum score of 199 is reflective of the most severe disability the result of PD (Holden et al., 2018). The MDS-UPDRS requires approximately 30 minutes to complete.
SEBR
SEBR was assessed by recording participant’s eye movements whilst sitting at rest. The recording device was located approximately 55cm directly in front of the participant. Participants were not informed that they were completing an assessment of their blink rate, nor were they engaged into conversation with the examiner as both informing participants that their blink rate is being assessed and conversing increase SEBR (Doughty, 2001). Participants eye movements were recorded for two-and-a-half minutes however, only the last one minute of each recording was coded for SEBR (one minute is sufficiently long enough to obtain a representative blink rate, Deuschl & Goddemeier, 1998). A blink was identified (and coded accordingly) as full eye lid closure which was the result of bilateral movement of the eyelids (Kimber & Thompson, 2000). SEBR was scored as the number of blinks per minute. PD participant pre-levodopa consumption SEBR was considered their baseline SEBR, reflective of intrinsic dopaminergic functioning (Kimber & Thompson, 2000).
Eye tracking tasks
Apparatus
A desktop mounted eye tracker (Eyelink Desktop 1000), operating in monocular mode, with a sampling rate of 500 Hz was used to record eye movements of the participant’s dominant eye. An adjustable chin rest with attached forehead rest was utilized to minimise head movements. The eye tracking camera was located at the base of the stimuli presenting computer monitor. Participants sat approximately 55cm away from the eye tracking camera and computer monitor. A 4-point calibration, whereby participants are asked to fixate upon a red circle as it moves from the top, bottom, right and left side of the computer screen, was used prior to the commencement of all eye tracking tasks. Frequent calibration improves the accuracy of eye-tracking data (Pi & Shi, 2019). All eye tracking tasks were developed and operated using experiment builder software version 1.10.1630. Habitual eye glass wearers were not required to remove their eyeglasses during eye tracking tasks. Eye tracking tasks required approximately 10 minutes to complete.
Prosaccade task
Participants completed four practice trials and 16 experimental gap trials. To centre a participant’s gaze at the start of each trial, a white fixation stimulus was presented for 1000 milliseconds (ms) in the centre of a back computer screen. A red lateralised target was then displayed randomly either to the right or the left of the central fixation for 1200ms at 4 ° eccentricity. The PS task operated according to the gap paradigm. Accordingly, to create a temporal gap between fixation and target stimuli, a black interval screen was presented for 200ms between the extinguishing of the white fixation stimulus and the presentation of the red target stimulus. For the PS task, participants were instructed to shift their visual focus towards the location of the red target as quickly and as accurately as possible.
Antisaccade task
Participants completed four practice trials followed by 24 experimental gap trials. Participants were presented with a white central fixation stimulus on a black computer screen for 1000ms. Following a 200ms black interval screen, a green lateralised target stimulus was presented at random to either the left or right of the central fixation. The green target was displayed for 2000ms at 4 ° eccentricity. Participants were instructed to shift their visual focus to the opposite direction of where the green target stimulus appeared. An example of a successful trial would be as follows, if the green target stimulus was presented left-lateralised, participants should direct their gaze to the right side of the computer screen.
Procedure
The present study was reviewed and approved by Lancaster University’s ethics committee. All participants provided informed consent prior to participating.
Participants were tested on one day and testing sessions took no longer than two hours. Individuals with PD completed SEBR assessments, MDS-UPDRS III motor examinations and all eye tracking tasks twice, once 30 minutes prior to consuming their usually scheduled dosage of levodopa medication, and once again one hour following the consumption of their levodopa medication. Prior research indicates that one hour is sufficient for levodopa to be metabolized and produce therapeutic effects (Lu et al., 2019). This method of testing the effect of anti-parkinsonian medications is widely used within the literature and no detrimental effects of this method have been reported (Cools et al., 2003). Similarly, re- test on the PS and AS tasks does not significantly influence performance (Larrison-Faucher et al., 2004). HC participants completed all study tasks once.
All participants completed the online questionnaire 48 hours prior to attending testing sessions. Upon arriving to testing, all participants completed an assessment of SEBR followed by the PS and the AS tasks. HC participants then completed the ACE-III and the Ishihara test. HC participation in the study was then complete. PD participants continued with further testing. Specifically, PD participants then completed the MDS-UPDRS subscale III motor examination. PD participants then consumed their usual dose of levodopa medication at their usual time. During the one-hour levodopa metabolization period, participants with PD completed subscales I, II and IV of the MDS-UPDRS, the ACE-III and the Ishihara test.
Once one hour had elapsed, individuals with PD then re-completed an assessment of SEBR, the PS and the AS task, and were also re-assessed via the MDS-UPDRS subscale III motor examination. Thus, motor symptom severity (MDS-UPDRSIII), SEBR and eye- tracking data were obtained from both pre (baseline) and post levodopa consumption medication states.
Data processing
Raw data were extracted via EyeLink using DataViewer Software Version 3.2 and processed offline using the bespoke software SaccadeMachine (Mardanbegi et al., 2019). SaccadeMachine removes noise and spikes within the data; frames with a velocity signal greater than 1500 deg/s or with an acceleration signal greater than 100,000deg2/sec are filtered out. Fixations and saccadic events were detected via the EyeLink Parser. Trials were excluded where participants failed to direct their gaze to the central fixation stimulus. To ensure saccadic data were reflective of responses to target presentation, a temporal window of 80-700ms from the initial onset of the target stimulus was used (i.e., anticipatory saccades produced prior to 80ms, and excessively delayed saccades produced after 700ms were excluded). The following variables were extracted from the processed data: PS latency (the time taken between the onset of the target stimulus and the first correct fixation), PS error rate (the number of times the participant failed to generate a reflexive saccade to fixate upon the target stimulus), AS latency (the time taken between the onset of the target stimulus and the first correct fixation in the opposite direction to the target stimulus), AS error rate (the number of times a participant erroneously performed a reflexive PS towards the novel target stimulus instead of looking away).
Publisher
Lancaster University
Format
Data/R.csv
Identifier
Austin 2022
Contributor
Rachel Jordan
Sian Reid
Sian Reid
Rights
Open
Relation
N/A
Language
English
Type
Data
Coverage
LA1 4YF
LUSTRE
Supervisor
Dr Megan Readman
Project Level
Msc
Topic
Neuro-clinical psychology
Sample Size
20 (9 individuals with mild-moderate Parkinson's disease, 11 healthy control individuals of similar age)
Statistical Analysis Type
Regression, T-Test
Files
Collection
Citation
Amy Austin, “Levodopa and antisaccade performance in Parkinson’s disease: the influence of intrinsic dopaminergic functioning, dopamine agonists and chronic anti-parkinsonian medication ,” LUSTRE, accessed January 30, 2026, https://www.johnntowse.com/LUSTRE/items/show/154.